
NOT WHAT THE DOCTOR ORDERED
Male teen endures long wait to address chest issue
After drawn-out process, insurer OKs surgery on enlarged breasts
8/25/2008
Dr. Kathy LaVorgna has encountered multiple, insurance-related frustrations in her efforts to gain approval to operate on the young man.
THE BLADE/JEREMY WADSWORTH
Buy This Image
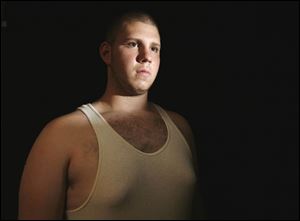
Panayiophs Tsiknis suffers from a disorder that causes boys to develop enlarged breasts because of an abnormal balance in hormones.
NORWALK, Conn. -- In their quest to convince insurers to cover the procedures prescribed by their doctors, patients with unusual conditions are finding more and more obstacles.
Panayiophs Tsiknis, an 18-year-old known as “Peter,” of Bridgeport, Conn., was asked to submit pictures of his enlarged breasts and participate in a psychological examination before his insurer, Anthem Blue Cross and Blue Shield of Connecticut, would even consider paying for an operation to have his breasts surgically removed.
Mr. Tsiknis’ physician, Dr. Kathy LaVorgna, said stories such as Peter’s “are constant, everyday stories” and she believes insurers are building barriers for patients in hopes that they will give in and not have operations prescribed by their physicians.
“That’s wrong,” said Dr. LaVorgna, the vice president of the Connecticut State Medical Society. “That’s a business decision only, and I swear they are trying to deny care for patients.”
On Thursday, after being contacted by The Blade earlier in the week for comment for this story, Anthem approved coverage for Peter’s operation.
“Anthem Blue Cross and Blue Shield in Connecticut has been awaiting specific information from the member’s physician that was needed in order to make a coverage determination,” Anthem spokesman Scott Golden said in a statement. “We just recently received the information we requested and based on that information, the treatment was approved.”
Peter’s surgery is now scheduled for Sept. 11, but getting the go-ahead from Anthem took months and months of denials and requests for more information.
READ THE SERIES: Not What The Doctor Ordered
For years, Peter longed for the day that he could rip off his shirt and run on the beach with his friends - free from shame, free from discomfort.
The teenager has a disorder called gynecomastia that causes boys to develop enlarged breasts often because of an abnormal balance in hormones. In most patients, the condition disappears during adolescence, but for others, such as Peter, it persists well beyond puberty, sometimes requiring surgery.
Despite pain from his enlarged breasts, Peter worked tirelessly to shed himself of the embarrassment.
He played baseball, basketball, and football. He worked with a personal trainer, lifted weights, did push-ups, and ran for miles each day. He changed his eating habits, opting for seafood and grilled chicken instead of greasy foods.
But no matter how much work he put in, Peter said: “My boobs - they stayed.”
Last year, after Peter’s 17th birthday, his mother took him to his pediatrician and then to Dr. LaVorgna. Dr. LaVorgna examined Peter and thought that with surgery, she could make his breasts appear normal.

Dr. Kathy LaVorgna has encountered multiple, insurance-related frustrations in her efforts to gain approval to operate on the young man.
Peter planned to have the operation on Feb. 17 during his winter break, but Anthem Blue Cross and Blue Shield said it wouldn’t pay for the surgery.
Dr. LaVorgna began working last year to get Peter’s surgery preauthorized by Anthem but encountered blockades and denials.
To get coverage for the operation, the insurer told Dr. LaVorgna she must prove that Peter was either 18 years old, which he wasn’t, or 18 months past puberty. With the teenager standing 6-feet-1 and weighing 255 pounds, Dr. LaVorgna, a surgeon for 19 years, felt confident telling the insurer that her patient was well past puberty.
The insurance company, however, rejected Dr. LaVorgna’s assessment of the teenager, saying she didn’t prove that the boy was 18 months past puberty. What was most perplexing to the doctor was that when she asked for the criteria for proving the teenager was 18 months past puberty, she said the insurance representative told her that no criteria existed.
“I said, ‘Do you understand what you just said to me?’ said Dr. LaVorgna, recalling her conversation with the insurance company. ‘You just said to me that I have to prove a criteria, but you don’t have the criteria that you want me to prove. That to me sounds like a no-win situation.’ “
Dr. LaVorgna - who performs a handful of gynecomastia-related surgeries each year and previously hadn’t experienced trouble gaining authorization from insurers - followed up her efforts with appeals to the insurance company, revisiting the American Society of Plastic Surgeons’ criteria for gynecomastia. But she repeatedly hit dead ends.
In a letter dated Feb. 8, 2008, Anthem’s utilization management department informed Dr. LaVorgna that Peter’s surgery would not be covered because it is not medically necessary for patients who aren’t 18 or are not 18 months beyond the end of puberty.
Instead of prolonging Peter’s battle with the insurer, Dr. LaVorgna eventually gave in and suggested he live with the condition until he turned 18. The patient and his mother begrudgingly agreed because they felt they had no other choice.
“So the kid has to suffer ... from 17 to 18, and I think that’s cruel,” Dr. LaVorgna said.
Said Peter’s mother, Marilyn Curwen, “It just prolongs the misery for him.”
On July 10, Peter turned 18. He scheduled his surgery for July 17, hoping to have plenty of time to recover before the start of his senior year of high school. He looked forward to tearing off his shirt in the locker room this fall without being ashamed.
But when Dr. LaVorgna tried to preapprove his operation, Anthem Blue Cross and Blue Shield provided a new layer of obstacles.
To be considered for coverage, Anthem said in a letter dated July 7 that Peter must first submit pictures of his enlarged breasts, the results of blood tests, and participate in a psychological evaluation within 45 days. Once Anthem receives the results of his testing, it will then decide whether it will cover his operation.
The reply caught Dr. LaVorgna by surprise because she felt the insurer said Peter wouldn’t face resistance if he scheduled the surgery once he turned 18.
Peter was skeptical that Anthem will ever cover his operation.
“It’s frustrating waiting and knowing that it might not happen,” Peter said last month before his insurer approved his surgery.
His dreams of returning to school for his senior year with a new body dashed, Peter is now looking forward to next summer. By then, he hopes to not only have had his surgery but be fully recovered in time to head to the beaches with his friends.
Contact Steve Eder at:seder@theblade.com or419-304-1680.