
GUEST COMMENTARY
Body’s reaction under microscope
How does the body fight bacterium that causes Lyme disease?
7/14/2014
A multiphoton laser scope used at the University of Toledo College of Medicine.
UNIVERSITY OF TOLEDO
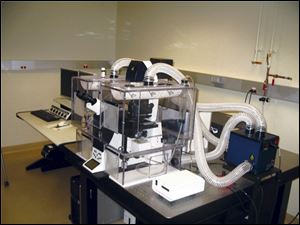
A multiphoton laser scope used at the University of Toledo College of Medicine.
This is one in a series of articles written by research students in the University of Toledo College of Medicine’s Biomedical graduate program exploring basic issues of human health.
How does the body fight bacterial infection once the skin is broken?
It’s similar to the way a town might come together in an emergency with everyone doing their part to repair damage and fight off invaders.
Using a special microscope equipped with a laser, my colleagues and I at the University of Toledo College of Medicine and Life Sciences have developed a method for documenting events that occur in the skin of a living animal after injury.
During an experiment, our research team sedates a laboratory mouse, pricks its ear skin with a needle and then views cellular activity at the injury site. Cutting-edge microscope technology allows us to produce 3-D videos of the events occurring at the wound site and define the behaviors of mouse cells as they occur in real-time. Since the mouse is simply asleep, it can be awakened and the experiment can be repeated several days later in the same animal to see the reaction to injury and healing process over time.

Lavik
While other scientists have witnessed some of these events previously using a similar technique, the UT researchers were the first to infect the skin injury site with the bacterium Borrelia burgdorferi and then visualize the response of immune cells using the microscope.
B. burgdorferi is the bacterium that causes Lyme disease following a bite from an infected tick. It has evolved to be very clever when in the skin and the immune system often has difficulty fighting the infection. Our technique for infecting the skin with this bacterium via a needle prick is very similar to how B. burgdorferi enters an animal naturally during a tick bite. Also, mice are one of the animals that the bacterium infects normally, making them an ideal model in the studies.
Using the microscope, UT researchers were able to witness many events typically hidden from the naked eye, such as how the mouse cells living just beneath the skin surface detect the injury within minutes of the needle prick. These cells produce chemical alarm signals that bring other cells to the injury site from all over the body and also provide them with instructions about how to behave and what to do. The specialized, first-responder cells are called neutrophils and through the microscope can be seen defending the immediate injury site and attempting to destroy bacteria as they cross the broken skin barrier.
The research also has allowed us to view other cell types, including macrophages, which assist in clearing damaged cells, and dendritic cells, which are named for their numerous arms resembling the branches of a tree. Such cells capture bacteria and carry them away.
While we did not view the lymphatic system in our experiments, we know that ultimately dendritic cells transport captive bacteria to lymph nodes where the bacteria are processed and presented to lymphocytes, another class of cells that circulate around the body. Some lymphocytes are better than others at targeting different types of bacteria. Thus, through examination of bacterial characteristics in the lymph node, lymphocytes with an expertise in fighting a particular variety of bacterium can be deployed out into the body on a search and destroy mission.
Through the experiments, UT researchers have found that B. burgdorferi is a sneaky organism. Not only does it move much more quickly than the neutrophils and dendritic cells that try to capture it in the skin, but it also seems to trick these cells into no longer seeing it as a threat. It is as if the bacterium camouflages itself and mouse cells perceive it as part of their normal environment, thus ignoring it.
If studies could find a way to impair this trickery, the body would likely be efficient at killing B. burgdorferi and fighting off Lyme disease. UT researchers are optimistic that their observations of how the bacterium and immune system interact will lead to improved therapies for those who develop this troubling illness.
John-Paul (JP) Lavik is a student who has recently earned both his Doctor of Medicine and Doctor of Philosophy degrees in the UT College of Medicine and Life Sciences' Biomedical Science Program. He is starting a pathology residency program at Yale University. He can be reached at john-paul.lavik@rockets.utoledo.edu. For more information, go to utoledo.edu/med/grad/biomedical.