
Health-care act's pre-existing condition program lacks money
Politicians bicker over fix as states halt enrollment
4/7/2013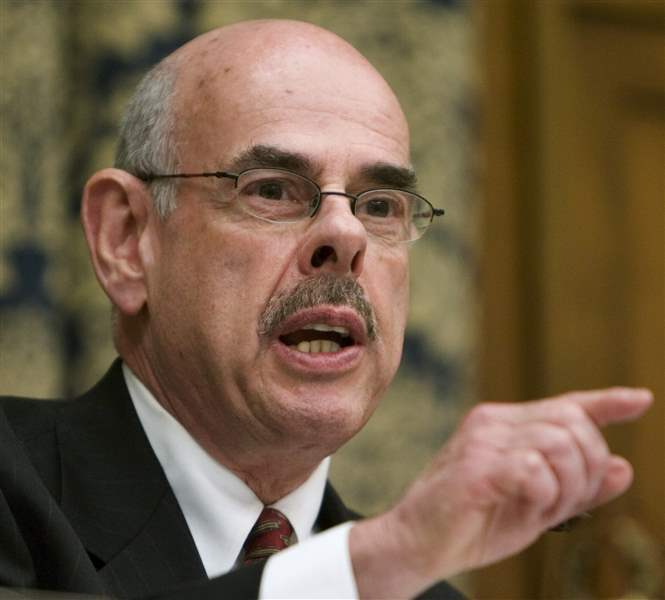
Rep. Henry Waxman (D., Calif.) says the program has been able to help the sickest Americans get treatment for costly and life-threatening conditions.
ASSOCIATED PRESS
Rep. Henry Waxman (D., Calif.) says the program has been able to help the sickest Americans get treatment for costly and life-threatening conditions.
WASHINGTON — Federal funding is running out for an Affordable Care Act program meant to provide temporary health insurance for people with medical conditions, forcing states to stop signing up new participants.
Critics say $5 billion was never enough to fund the Pre-Existing Condition Insurance Program, or PCIP, and that financial problems were exacerbated by over-representation by people with very serious medical conditions that are expensive to treat.
Even conservatives who want to repeal the Affordable Care Act say the PCIP provision wasn’t funded well enough. Coverage of medical conditions is one of the few objectives of the Affordable Care Act that Republicans and Democrats agree on.
“These people are sick. They have multiple medical conditions” that are costly to treat, U.S. Rep. Michael Burgess (R., Texas) said.
Mr. Burgess said Congress should have appropriated $30 billion for the program. That cost would be “but a drop in the bucket compared to the whole Affordable Care Act,” he said during a congressional hearing last week.
Now he and other House Republicans want to fill the gap by transferring funds from other parts of the Affordable Care Act. Supporters of the act, though, say such a move would only undermine the architecture of broader health reform set to take effect in January.
About 135,000 people nationwide signed up for PCIP before the federal government shut down enrollment last month, saying there wasn’t enough money to continue. Some individual claims had run as high as $225,000.
Just 4.4 percent of people enrolled account for half the claims paid, according to the Commonwealth Fund, a private foundation that advocates for access to health care.
Coverage will continue for people already enrolled, but they now face higher costs. Because of the funding crunch, their maximum out-of-pocket spending limit increased from 4,000 to $6,250.
The U.S. Department of Health and Human Services said 3,380 Ohioans were enrolled in the program, while 2,204 were enrolled in Michigan through Jan. 31.
The enrollment suspension is bad news for people with medical conditions who have been turned away by private insurance companies or charged exorbitant premiums.
Susan Zurface, 42, of Hillsboro, Ohio, is among those turned away. The attorney wasn’t carrying health insurance in January when she was diagnosed with chronic lymphocytic leukemia and almost immediately racked up $60,000 in medical bills. Now, she says, her options for paying for treatment are limited.
She isn’t healthy enough to be able to get affordable insurance in the private market and isn’t sick enough to qualify for Medicaid coverage for the disabled.
“Without the benefit of coverage, I will be willfully incurring expenses that I know I have no means to pay, in which case, I will have to consider bankruptcy to discharge whatever medical expenses I have incurred from providers who treated me in good faith, but whom I cannot pay for their services,” said Ms. Zurface, who testified before the Health subcommittee on behalf of the Leukemia & Lymphoma Society.
She said she hoped Congress would find a way to reinstate the program and to improve it by reducing premiums and removing a requirement for participants to be uninsured for six months before they can be eligible.
House Republicans, including subcommittee Chairman Joe Pitts of Pennsylvania, were quick to blame poor planning by the Obama Administration and underfunding by congressional Democrats who crafted the Affordable Care Act. During debate over the 2010 Affordable Care Act, Republicans had wanted to spend $25 billion for the line item.
Before the act, insurers treated people with medical conditions unfairly, and the consequences have been dire, Families USA Executive Director Ron Pollack testified Wednesday before the House Energy and Commerce Subcommittee on Health.
He said he is very concerned that the stopgap PCIP was suspended.

Lt. Gov. Mary Taylor, who runs Ohio's insurance department, says the federal government has done a poor job managing the program.
Ohio Lt. Gov. Mary Taylor, who runs her state’s insurance department, said federal requirements took flexibility from more effective state programs that provided coverage.
Last week, she told the House Energy and Commerce Subcommittee on Health that the federal government has done a poor job managing PCIP and that she fears the problems are a harbinger of trouble to come as the core provisions of the Affordable Care Act take effect next year.
“These fears are very real and post a threat not just to regulation of health insurance in Ohio but across the country,” she told subcommittee members.
Health policy analysis have expressed concerns that the PCIP funding shortage is evidence that the federal government may have underestimated the cost of insuring others who will enter the market in January when coverage mandates take effect.
The program for high-risk people was meant as a stopgap to January, 2014, when permanent subsidies are scheduled to begin.
The program has provided transitional support for people otherwise uninsurable in the individual insurance market, but its limitations demonstrate why high-risk pools aren’t adequate substitutes for comprehensive reforms that will go into effect in January, said Sara Collins of the Commonwealth Fund.
By mandating coverage and eliminating medical exclusions, the reforms will spread risk over a larger pool, she told the subcommittee.
“A shared responsibility across the population and the lifecycle is essential for an equitable and efficiently run health insurance system,” she testified.
Thomas Miller told subcommittee members that the provision was a “poorly designed, half-hearted gesture within the ACA, aimed primarily at minimizing political risks rather than addressing a serious problem.” Mr. Miller is a health-policy researcher and a resident fellow at the American Enterprise Institute, a right-leaning Washington think tank.
Rep. Henry Waxman of California, ranking Democrat on the subcommittee, defended the provision. It has been able to help the sickest Americans get treatment for costly and life-threatening conditions, wrote Mr. Waxman, who did not attend the hearing.
“Expanding access to coverage and efficiently [spreading] risk across the market is a far better solution to the problem of rampant uninsurance and pre-existing condition exclusions than locking sick Americans into increasingly expensive coverage through high-risk pools,” Mr. Waxman wrote. “If my Republican friends truly share the goal of caring for sick and chronically ill Americans, they will work with us to ensure a smooth transition to 2014 rather than attacking PCIP.”
Ohioans being turned away from the federal plan are still eligible for a state-run alternative.
Block News Alliance consists of of The Blade and the Pittsburgh Post-Gazette. Tracie Mauriello is the Post-Gazette’s Washington bureau chief.
Contact her at: tmauriello@post-gazette.com, 703-996-9292, or on Twitter @pgPoliTweets.